Uncertain Health in
an Insecure World – 41
“Innovation
Orientation”
Orientation determines our point-of-view and related actions.
Physicians are trained to determine whether or not a patient
is oriented to “person, place and time”.
“Who are you?” Where
are we?” What day is it?”
These three simple questions are fundamental to obtaining an
accurate medical history, in that those patients who are not “oriented x3” are a danger to themselves,
and possibly to others.
Once a patient’s orientation is established, effective
humanistic medical care can be delivered. In this way, and as recited in the
Hippocratic Oath, the medical profession aspires to “do no harm”.
This month, over 20,000 young MD’s will graduate from North
American medical schools. Each new doctor will possess this clinical skill, among
others. The same is true of over 100,000 other medical graduates around the
globe.
Entering the health professions workforce requires that
certain basics be mastered, before the complexities of healthcare delivery can even
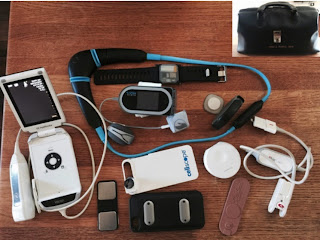
be contemplated. As the modern devices & handheld tools show (below), modern medicine is creative and innovative.
But healthcare is not some clever game! And old Hippocrates still advises modern physicians to step away from the patient if they feel their skills have been exceeded.
But healthcare is not some clever game! And old Hippocrates still advises modern physicians to step away from the patient if they feel their skills have been exceeded.
But how are innovators oriented?
Who decides when incubees are ready to graduate? What are
the basic innovator skills? Where does the innovation workforce train up? Just
what are the real world implications of being under-prepared when entering the
innovation sector – on personal careers and on an entire business?
We have previously addressed the “Innovation Concentration”—the enrichments that foster success in
the Silicon Valley (see post #27). In
the absence of that unique California innovation ecosystem (or an oath that
demands deep professional reflection), just how is innovation’s “harm” mitigated? How is the public
interest protected?
First, let’s all agree that change per se is not always healthy. And whether incremental or disruptive,
innovation is not de facto always
positive.
What is the
general state of health for business innovation?
·
A 2010 Capgemini survey of global executives
reported that only 11% of business innovations had a positive financial impact
at least 75% of the time.
·
A 2013 Accenture survey of CEO’s found that only
18% of business innovations produced a tangible payoff, and that only 4%
recovered the cost of capital invested.
Business models exist to objectively evaluate health status,
healthcare access and health system financing. As health and healthcare systems
demands increase, the pressure for business innovation grows. Healthcare
delivery and insurance leaders are generally risk averse when considering
expansion and bundling decisions. The desired outcome should be better health –
increased wellness and decreased illness – underpinned by the social contract of
healthcare system sustainability.
But is innovation really happening?
Recently, Harvard Global Health and Population professor Peter Berman purposefully differentiated
health systems from healthcare delivery systems at the University of California
Berkeley Global Health Leadership Forum. In both systems, he noted that, “Change
is a constant… driven by new
needs and technologies… (based on) recent gains to build upon. Change must
improve consequences like health outcomes, not
just reorganize”.
Simply put, real health innovation is not just healthcare system change!
Ironically, sometimes the health systems of the poorest global
economies prove themselves to be the most innovative – rehydration,
short-course TB therapy, antibiotics for childhood acute lower respiratory infection, India’s decade old National Rural Health Initiative are some
examples. Chaotic out-of-pocket spending is becoming organized and captured by
payment systems.
For doctors, the possible etiologies of a patient’s acute
illness fall under the medical term “differential
diagnosis”. Make the right diagnosis, and the patient recovers. Make the
wrong diagnosis, and the patient develops a chronic illness… or dies. Doctors have more innovative tools in their doctor bags.
For healthcare leaders, an entrepreneur’s wish list of
potential breakthroughs is called “opportunities”
– genetic testing, telemedicine, novel biotech drugs, integrated care and
personalized medicine. Well-informed business and policy decisions can
accomplish true innovation. But in this setting, acting without discipline or in
the absence of analytics produces change… only change.
When doctors violate the Hippocratic Oath and cause “harm” to their patients, they should be
sanctioned by others in the medical profession.
Innovators lacking the business basics may also cause “harm”. In the under-regulated innovation
space, the damage done often goes unsanctioned by others, or worse,
unrecognized by all.
So, just like a medical school curriculum covers the basics,
a comprehensive and consistent analytic framework is needed to evaluate models
of purported innovation.
Reorganization by change alone, without true innovation and
related outcomes, can be frankly disorienting. And like a disoriented patient,
this is potentially dangerous!
Those of us in the Square who train doctors and try health innovation appreciate the
difference.



No comments:
Post a Comment