Uncertain Health in
an Insecure World – 50
“Digital House Call”
As early as 1925, “diagnosis by radio” was predicted in Science and Invention magazine. I recall watching the 1959 television series, The
Flying Doctor, inspired by the Royal Flying Doctor Service of Australia. Dr.
Greg Graham (played by Richard Denning) flew into the remote outback, serving
the medical needs of inhabitants and Aboriginal peoples.
Given the option,
most patients would rather be seen face-to-face by their physician. But population
growth in the developing world and chronic physician shortages in developed
countries mean there are tens of millions who simply cannot see a doctor in the
flesh.
That is uncertain health. That is an insecure world.
That is uncertain health. That is an insecure world.
The telehealth era
began at the Medical College of Georgia in 1993. As the immediate past dean, I
am proud that the electronic house call was invented there by Dr. Jay Sanders. The
U.S. Institute of Medicine released a definition and made recommendations
in 1996. It has since evolved into the standard of care for healthcare access
by millions. Governments around the world are actively pursuing efforts to
get people onto the telehealth grid (like Inuits, below).
Telehealth (a.k.a. telemedicine, e-health or
e-medicine) is the all-inclusive term for virtual care delivery at a distance. Communications take place between physician
and patient or between physician and consultant, either in real-time or
asynchronously using “anytime” store
& forward capabilities. Only real-time care meets U.S. Medicare’s narrow
definition of reimbursable telehealth services.
At the just completed
2015 Global Telehealth Conference in Toronto, the theme was “serving the
underserved”. Scientific papers from >25 countries showed that telehealth
technology is continuing to make a difference in global healthcare. Telehealth
is widely utilized for stroke management in a hub & spoke model, with
systems like the Mayo Clinic at the center of the wheel. In novel ways,
telehealth is now the basis for virtual tumor boards, diabetes population
management and retinal scanning (above), and off-site ICU patient monitoring. Ebola
patient Dr. Richard Sacra (below), in quarantine in Nebraska and physically separated
from family and doctors for bio-containment purposes, was cared for using the Vidyo telehealth platform!
The global telehealth
market will double in the next five years at a robust CAGR of 18.9% through
2019. This sector is receiving intense VC interest and major vendor
investments, including big plays by McKesson, GE, Seimans, and Philips
Healthcare. IHS Inc. predicts that the U.S. telehealth market will grow by
50% per year to US$1.9B in 2018.
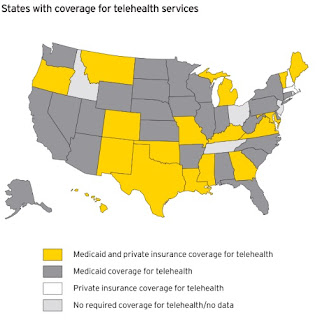
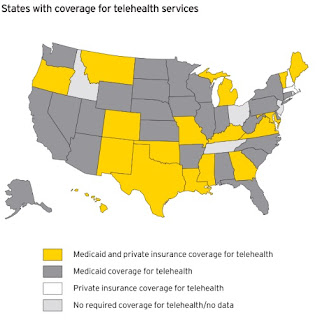
Much of the impetus
for such rapid growth comes from U.S. healthcare reform requirements for
universal access and pressure to expand population health management.
Increasingly, U.S. states are authorizing payments for telehealth services in
public programs and for privately insured patients in 24 states and the
District of Columbia. More than 50% of U.S. hospitals now use some form of
telehealth platform. Deloitte predicted that in 2014, 75 million of the 600
million G.P. visits in the U.S. and Canada would be e-visits.
One wonders how this well-aging,
fixed platform telehealth tortoise will keep pace with the newer, more nimble
digital health, AI, IoT and robotic hares. Increasingly, the tools of
telehealth are digital and portable – laptop webcams, video-enabled
smartphones and tablets.
Several large employers
such as Booz & Co., Home Depot and Westinghouse Electric now offer
telehealth consultations to their employees. Walgreens Boots Alliance, Inc. is
now collaborating with MDLIVE to
expand their digital telehealth offerings in pharmacies located states like
Colorado and Washington. In 2015, Walgreens Boots and MDLIVE jointly launched a mobile app for iOS and Android devices to
connect customers 24/7 with board-certified doctors. Walgreens just announced
that this service will be available in 25 states by the end of 2015.
Is there anything
that t
Dr. Peter Antall, CEO
of Online Care Group, warns that telehealth should not “disintermediate care from one’s medical home, particularly their
primary care.” In June, the pro-doctor American Medical Association (AMA)
tabled its ethical guideline for telehealth services due to delegates’ concerns
about AMA guidelines requiring an initial face-to-face patient-doctor visit.
Previously, AMA had required that telehealth doctors be licensed in the
patient’s state.
There’s little risk
of people living near doctors becoming telehealth shut-ins.
Telehealth brings certainty to an insecure world,
Telehealth brings certainty to an insecure world,
We in The Square don’t
want doctor disintermediation, especially when the human touch is part of
healing. But technology is progress, and by bringing care everywhere, telehealth
is the next best thing.






No comments:
Post a Comment